The entry-level Doctor of Occupational Therapy (OTD) degree program is accredited by the Accreditation Council for Occupational Therapy Education (ACOTE) of the American Occupational Therapy Association (AOTA) located at:
7501 Wisconsin Avenue, Suite 510E
Bethesda, MD 20814
(301) 652-AOTA
www.acoteonline.org
Program Description
The entry-level OTD program is a lockstep, full-time program that takes three years to complete. It is a 100-credit-hour program designed to be completed in nine consecutive semesters. Students complete the didactic and laboratory portion of the curriculum during the first two years of the program on the Lubbock TTUHSC campus. These courses prepare students with the critical reasoning, professionalism, and practice skills necessary for an evidence-based practice that is grounded in occupational therapy theory. Students will also begin preliminary courses related to their doctoral capstone during the second year of the curriculum.
During the third year of the program, students will complete 24 weeks of level II fieldwork education, their doctoral capstone project, and a 14-week doctoral capstone experience. With admission criteria, the total time to earn the OTD degree equals a minimum of six full-time equivalent academic years (i.e., the three-year OTD curriculum and the admission criteria of an earned bachelor’s degree).
Students are required to adhere to all program, departmental, and school policies as outlined in the student catalog, student handbook, course syllabi, fieldwork manual, and doctoral capstone manual.
Successful completion of the program leads to a Doctor of Occupational Therapy (OTD) degree. Graduates of the program will be eligible to sit for the National Certification Examination for the Occupational Therapist administered by the NBCOT. After successful completion of this exam, the individual will be an Occupational Therapist, Registered (OTR). In addition, all states require occupational therapists to have state licensure in order to practice. Licensure requirements vary by state according to the practice act and state regulations that govern the practice of occupational therapy; however, state licensure is usually based on the results of the NBCOT certification exam. A criminal conviction (e.g., felony or misdemeanor) may affect a graduate’s eligibility to take the NBCOT Certification Examination or attain state licensure.
OTD Vision
To earn recognition for elevating the practice of occupational therapy by promoting our distinct value as clinicians and professionals.
OTD Mission
To provide students with a strong foundation in professionalism, critical reasoning, and practice skills to become competent occupational therapists who use meaningful occupations to help people improve their health and well-being.
Philosophy Statement
The value of a profession lies within its professional identity and its distinct contribution to society. A deep understanding of the profession’s core subject is critical for the development of a strong professional identity and articulation of the profession’s distinct values. The core subject of the occupational therapy profession is the dynamics of occupation. Dynamics of occupation is a construct that characterizes how engagement in meaningful, necessary, and familiar activities (i.e., occupation) affects a person’s health and well-being. Dynamics are forces that influence growth, development, or change within a system or process. The dynamics of occupation can be understood as the forces related to occupational engagement that impact health and well-being.
Occupational therapists believe that being occupied in meaningful, necessary, and familiar activities is a source of health and well-being for human beings. These activities, or occupations, encompass areas that include: self-care, learning, work, play, leisure, social participation, and sleep/rest. Each person has a unique configuration of meaningful occupations that relate to their roles, habits, routines, contexts, and environments. Various life circumstances and health conditions can disrupt a person’s ability to engage in valued occupations.
Occupational therapists use their understanding of the dynamics of occupation to provide occupational therapy interventions that help people do the day-to-day activities that are important and meaningful to them. Occupational therapists work collaboratively with individuals, families, caregivers, and other groups whose life patterns and abilities to engage in valued occupations have been altered for various reasons (e.g., cognitive or developmental problems, injury or illness, social or emotional deficits, aging process). Occupational therapists apply critical reasoning and practice skills as they evaluate, plan, facilitate, and reflect on client care. The distinct value of occupational therapy is to improve health and well-being through facilitating participation and engagement in occupations at home, school, workplace, community, and various other settings.
Occupational therapy education must provide opportunities for students to integrate a wide range of topics learned to the core subject—dynamics of occupation—so that students profoundly understand and clearly articulate the distinct value of occupational therapy. Developing a deep understanding of the dynamics of occupations requires that students:
- Learn what constitutes an occupation and how to analyze activity demands
- Learn how to assess a person’s unique occupational profile
- Learn how to analyze occupational performance
- Learn how occupations can be disrupted, impoverished, or changed over time
- Learn how underlying neurological and physiological mechanisms that positively and negatively affect occupational engagement, performance, and participation
- Learn therapeutic strategies, techniques, and activities to help people engage, perform, and participate in meaningful occupations
- Learn methods to evaluate changes in occupational participation, health, and well-being
Curriculum Design of the OTD Program
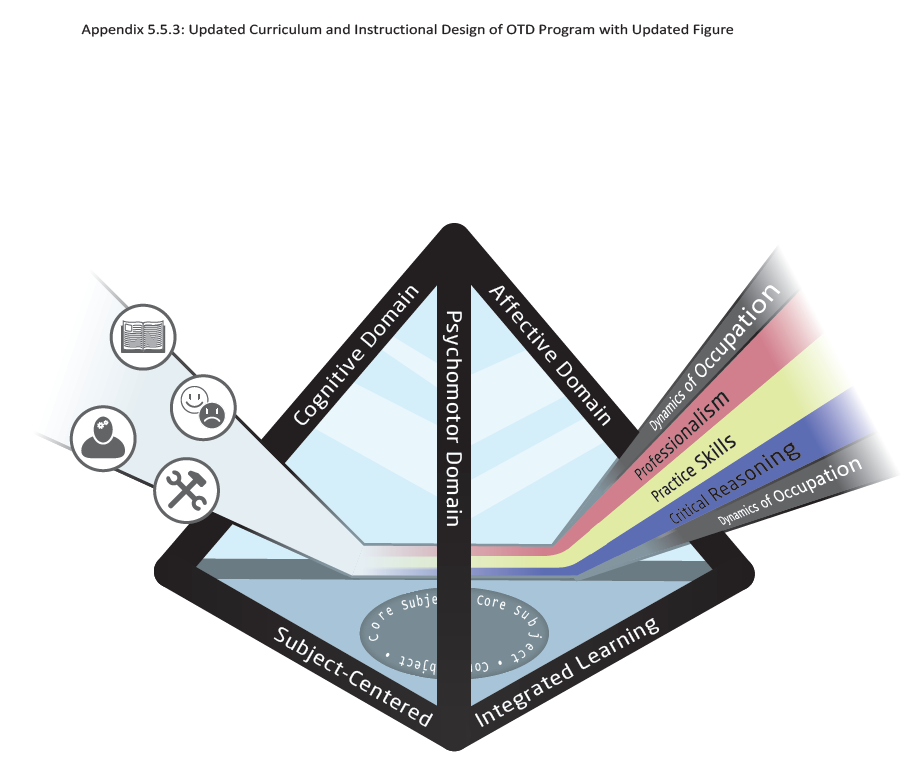
The curriculum design has four major content areas (i.e., curriculum threads) that are apparent throughout the curriculum. These are the dynamics of occupation, professionalism, critical reasoning, and practice skills.
Dynamics of Occupation
The core subject of the occupational therapy profession is the dynamics of occupation. Dynamics of occupation is a construct that characterizes how occupation—engagement in meaningful, necessary, and familiar activities—affects a person’s health and well-being. Dynamics are forces that influence growth, development, or change within a system or process. The dynamics of occupation can be understood as the forces related to (or facilitating) occupational engagement that impacts health and well-being.
Professionalism
Students learn key concepts related to being a professional who is prepared to be a self-directed lifelong learner; to uphold ethical standards, values, and attitudes of the profession; to effectively communicate and work interprofessionally with others; and to demonstrate active involvement in professional development, leadership, and advocacy.
Critical Reasoning
Students learn key concepts related to being a critical thinker who demonstrates the ability to synthesize information necessary for the development and implementation of theory-driven, evidence-based occupational therapy interventions.
Practice Skills
Students learn key concepts related to being a competent practitioner who can apply evidence-based evaluations and interventions to address physical, cognitive, psychosocial, and sensory aspects of performance in a variety of contexts and environments to support occupational engagement and participation.
Curriculum and Instructional Design
The figure below presents a model of the program’s curriculum design. The pyramid illustrates how the curriculum design provides a framework to facilitate the transformation of the student’s knowledge, skills, behaviors, and attitudes throughout the program. The base of the pyramid illustrates the SCIL-OT framework and how the core subject (i.e., Dynamics of Occupation) is foundational to the curriculum and instructional design. The three sides of the pyramid illustrate Bloom’s Revised Taxonomy framework and how the three domains of learning (i.e., cognitive, psychomotor, affective) are included in instructional design. The beam of light represents the transformation of student learning throughout the curriculum with the recognition that students enter the program with knowledge, skills, behaviors, and attitudes as represented by the icons on the left side of the pyramid. The beam of light traveling through the pyramid represents the development of students’ professionalism, practice skills, critical reasoning, and understanding of the profession’s core subject (i.e., dynamics of occupation). These four concepts form the curriculum threads that are introduced and integrated throughout the curriculum to guide student learning and development. The curriculum threads structure the scope of the curriculum content and how the core subject (i.e., dynamics of occupation) is integral to each of the other curriculum threads. The transformation yields achievement of student learning outcomes in the areas of critical reasoning, professionalism, practice skills, and dynamics of occupation as depicted by the beam exiting the pyramid on the right.
Fieldwork
Fieldwork education is an integral aspect of our program. Students will be involved in Level I Fieldwork experiences during the first and second years in the program. Students complete 24 weeks of full-time Level II Fieldwork during the third year of the program. Students must complete all Level II Fieldwork within 12 months following the completion of the didactic portion of the curriculum. Level II Fieldwork courses are typically full-time and will often require the student to relocate outside the immediate geographic area. In rare situations, a Level II Fieldwork experience may be completed on a part-time basis to meet a student's accommodation requirements or extenuating circumstances.
Fieldwork education consists of the following experiences designed to prepare and expose the student to a variety of applied settings in occupational therapy:
- Level I experiences in pediatrics occur in association with HPOT 6240 Intervention: Developmental and Learning Models II in the Summer 2 semester. The student will actively participate in faculty-led learning experiences within the community to develop professional and therapeutic skills with the pediatric population.
- Level I experiences in mental health occur in association with HPOT 6240 Intervention: Cognitive and Behavioral Health Models in the Summer 2 semester. The student will actively participate in faculty-led learning experiences within the community to develop professional and therapeutic skills addressing behavioral, psychological, and social factors influencing engagement in occupation.
- Level I experiences in adult physical dysfunction occur in association with several courses over the first and second year. Integrated within these select courses, students apply knowledge to practice through participation in progressive comprehensive competency experiences relevant to practice in adult settings and understanding the needs of clients. Specific therapeutic competency experiences include the progressive use of simulated environments and standardized patients.
- Fieldwork II 1: This full-time fieldwork experience typically begins in May of the third year and lasts 12 weeks. The student engages in an in-depth experience delivering occupational therapy services to clients, focusing on the application of purposeful and meaningful occupation, administration, and management of occupational therapy services.
- Fieldwork II 2: This full-time fieldwork experience typically begins in August of the third year and lasts 12 weeks. The student engages in an in-depth experience delivering occupational therapy services to clients, focusing on the application of purposeful and meaningful occupation, administration, and management of occupational therapy services. At least one of the two Fieldwork II experiences must be in an adult physical dysfunction setting. The other Fieldwork II experience may be in a different adult setting, a pediatric setting, mental health setting, or other specialist settings (e.g., hand therapy; neuro specialty).
Facilities that have occupational therapy clinical education agreements with TTUHSC may be used for Fieldwork sites. The Academic Fieldwork Coordinator provides detailed information for selection procedures. The student may provide preferences for certain setting types and for the location of Fieldwork II placements. The program has opportunities locally, across the state, and in other states across the US.
Doctoral Capstone
An integral part of the program curriculum, the Doctoral Capstone (DC) provides in-depth exposure to one or more of the following areas:
- administration and leadership,
- program development,
- education,
- clinical practice skills,
- research skills,
- advocacy,
- and theory development.
It consists of two parts: (1) the capstone experience and (2) the capstone project.

*Areas of program emphasis/specialty.
Doctoral Capstone Experience (DCE)
The DCE develops occupational therapy students in one or more of the DC areas. The DCE occurs at a mentored practice setting known as the DCE site. The Doctoral Capstone Coordinator (DCC) will collaborate with the student to establish the DCE site and the required written memorandum of understanding. During the DCE, the student is mentored by an individual with expertise consistent with the student’s DC area of focus. This mentor, known as the DCE site supervisor, does not have to be an occupational therapist. More than one student may be present and working collaboratively at the DCE site at the same time; however, each student has individual capstone objectives and focus.
The 14-week (560 hours) DCE, beginning in January of the third year, must be completed after completion of all coursework, Level II fieldworks, and required preparatory activities (i.e., literature review, needs assessment, goals/objectives, and evaluation plan). Students must complete the final doctoral capstone course within 6 months following the completion of Level II fieldwork. No more than 20% of the 560 hours can be completed on work outside the objectives of the capstone site. The DCE is NOT a third Level II fieldwork. As such, the student will identify goals and objectives, requiring approval in advance of the DCE, to achieve the identified in-depth experience. The objectives for the DCE will overlap with the capstone project objectives; however, additional objectives and tasks specific to opportunities within the DCE site will also be developed. All DCE sites are located in the Lubbock area.
Doctoral Capstone Project (DCP)
The DCP develops occupational therapy students' capacities to engage in scholarly activities. The student completes an individual culminating product to demonstrate synthesis and application of knowledge gained in one or more of the DC areas. The DCP is a highly student-driven process; however, the student works in collaboration with a faculty capstone mentor and possibly a DCE site supervisor to develop a plan to achieve individualized learning objectives and produce evidence of scholarship.
The student engages in preparatory activities for the DCP during coursework and prior to the DCE that includes a literature review, needs assessment, goals/objectives, and an evaluation plan. The student must have an approved DC proposal prior to beginning the DCE. The student then engages in scholarship that supports the DCP during the DCE. Following the DCE, the student finalizes and disseminates their DCP. Examples of products that may document this scholarship include an educational presentation, case report, treatment manual, curriculum, grant proposal, quality improvement project report, program proposal, or resource portfolio. Capstones requiring IRB processes will only be granted on joint projects with academic/professional research teams. The student presents their DCP at the TTUHSC OTD Scholarship Symposium prior to graduation.
Technical Standards
The Occupational Therapy program at Texas Tech University Health Sciences Center (TTUHSC) is a rigorous and intense program that places specific professional, intellectual, physical, and social requirements and demands on the students enrolled in the program. An objective of this program is to prepare graduates to enter a variety of employment settings and to render care to a wide spectrum of individuals with physical and psychosocial impairments. The technical standards set forth by the occupational therapy program establish the essential qualities considered necessary for students admitted to this program to achieve the knowledge, skill, and behavioral competencies for entry-level practice. These standards are subject to amendment based on changes in health care and the scope of occupational therapy practice.
The ability to meet these technical standards is required for admission to the Occupational Therapy program and must be maintained throughout the time a student is enrolled in the program. Applicants to (or accepted applicants for) the Occupational Therapy program will be required to verify that they understand and meet these technical standards, or that they believe that with reasonable accommodations they can meet the technical standards.
In keeping with applicable federal and state law regarding disabilities, we are committed to making reasonable accommodations for students with disabilities to enable them to perform successfully in our program. Any student with a disability who is accepted to the Occupational Therapy program must contact Student Disability Services (SDS) in the TTUHSC Office of Student Affairs as soon as possible. SDS Staff will determine whether the stated condition qualifies as a disability under applicable laws and work with the program faculty to determine reasonable accommodations.
There are two separate and distinct components in the curriculum for the Occupational Therapy program: 1) an academic didactic component, and 2) a clinical/fieldwork component. Accommodations in place for the didactic component may not be the same accommodations available for the clinical component in the curriculum. The technical standards listed below are necessary functions and skills for the development of the knowledge, skills, and behaviors to provide safe and effective occupational therapy services.
- Cognition:
a. Applicants and students must be able to skillfully conceptualize, apply, analyze, synthesize, and evaluate information from a broad range of sources. The use of these learning domains must produce effective critical thinking skills to be used during observations of patient behavior, task performance, and the environment. To produce the required didactic and clinical learning, students must have:
- Sufficient perception and attention (sustained, shifting, and divided) to perform components, such as discernment and discrimination of relevant information (e.g., attention to safety concerns during laboratory and clinical/fieldwork experiences; sustained attention for actively learning during lectures and taking tests lasting up to 4 hours); accurate perception and interpretation of spatial relationships (e.g., surface anatomy; analysis of movement); and acquisition and use of knowledge within rigorous time constraints (e.g., assignment due dates, semester schedules, allotted treatment time).
- Sufficient memory skills (immediate, short term/working, and long term) to perform components such as the transfer of immediate memories (from sensations) to short term memories, which are then developed into long term memories through various learning strategies. All forms of memory should be accessible/retrievable for use in working memory as evidenced by effective didactic and safe and effective clinical experiences (e.g., assignment completion; examination preparation; occupational therapy evaluation; treatment planning; reassessment; outcomes review).
- Sufficient higher-level cognitive skills to perform components, such as concept formation (e.g. development of theoretical concepts in occupational therapy); cognitive flexibility (e.g. understanding of various contexts and patient situations); problem-solving and decision making (e.g., searching and evaluating published literature; selection of appropriate assessments and treatment strategies); and accurate self-assessment of clinical/fieldwork skills, professionalism, and academic performance (e.g. monitor one’s own actions; learn from peer, instructor, client, and environmental feedback).
- Communication:
a. Applicants and students must be able to effectively communicate with a broad range of individuals, such as peers, faculty, patients, caregivers, family members, other professionals, supervisors, and payers. Such communication requires that students can effectively engage in receptive and expressive forms of communication (e.g., written, spoken, non-verbal). Students must have:
- Sufficient proficiency with the English language to perform components, such as the acquisition of information and knowledge through written and spoken language (e.g., classroom instruction, textbooks, journal articles, websites, videos); production of written assignments with accurate spelling, grammar, and writing mechanics (e.g., essays, documentation); completion of examinations that require reading and comprehension; and professional presentation of information (e.g., class presentations; interdisciplinary team discussions; patient status reports).
- Sufficient proficiency with the use of technology to perform components, such as the utilization of computer resources for didactic, laboratory, and clinical/fieldwork courses (e.g., internet, email, electronic health records, and computer software for word processing, spreadsheet, and presentation); accessing content using a variety of electronic media (e.g., videos, pdf, forums, electronic library databases); and utilization of technology resources used for standardized testing (e.g., electronic modalities).
- Motor Skills:
a. Applicants and students must be physically capable to perform a range of motor skills. Such motor skills require functional movement to effectively perform various physical components of patient assessment and intervention. Students must have:
- Sufficient muscular and cardiovascular endurance to perform components such as positioning and stabilization of patient; and sustaining physical activity levels necessary to meet academic and clinical/fieldwork productivity (e.g., classroom and clinical/fieldwork activities)
- Sufficient fine motor coordination, range of motion, and strength to safely perform components, such as grasp and manipulation of therapy supplies, tools, and equipment (e.g., cut and form materials to fabricate splints and assistive devices; positioning of supplies or equipment in accordance with standardized testing procedures); demonstration of dexterous movements for various activities of daily living (e.g., write, button, open containers); and application and calibration of pressure to soft tissue (e.g., massage, facilitation, inhibition, and handling techniques).
- Sufficient gross motor coordination, range of motion, and strength to safely perform components, such as stabilization, positioning, and moving of patient (or patient’s body parts); maneuvering patient in a wheelchair; application of physical resistance to assess muscle strength and tone; and accommodation and/or demonstration of the desired positioning or movement patterns for the patient (e.g., crouch, kneel, squat, bend, reach, sit).
- Observation:
a. Applicants and students must be able to effectively observe behavior, task performance, and the environment. Such observation requires the functional use of their senses. Students must have:
- Sufficient vision acuity and perception to perform components such as visual observation of educators and/or peers demonstrating techniques, procedures, and equipment use; seeing and reading text and images( e.g., equipment gauges/dials, medical records); observation of patient behaviors, skills, and impairments; visual inspection of signs of distress, trauma, or impairment; visual monitoring of tools and equipment for safe, effective operation; and identification of environmental barriers and supports.
- Sufficient auditory function to perform components, such as hearing patient’s verbalizations and utterances; monitoring of tools and equipment for safe, effective operation; and accurately hearing sounds from the pulmonary, cardiovascular, gastrointestinal, and musculoskeletal systems.
- Sufficient tactile sensation to perform components, such as accurate discernment, palpation, and mobilization of muscles, bones, joints, and other subcutaneous structures; monitoring of temperature or tension through touch; and manipulation of supplies, tools, and equipment.
- Social Behavioral Skills:
a. Applicants and students must be able to establish and regulate behaviors to meet the performance demands of occupational therapy practice. Such social behavioral skills require motivation, self-awareness, emotional regulation, and interpersonal skills. Students must have:
- Sufficient motivation to achieve academic or clinical/fieldwork performance expectations that include components, such as self-direction and autonomy (e.g., utilize organization and time management skills; utilize resources for self-directed learning; access transportation to attend academic courses and clinical/fieldwork placements); compliance with academic and professional standards of conduct (adhere to safety guidelines and procedures; conduct oneself in an ethical and legal manner); and portrayal of honesty, integrity, and professionalism in all circumstances.
- Sufficient interpersonal skills to perform components, such as respect for individual, social and cultural diversity; building and maintaining healthy relationships with a broad range of individuals (e.g., peers, faculty, patients, caregivers, family members, other professionals, and supervisors); facilitation of therapeutic interaction (e.g., attending, clarifying, coaching, facilitating, and touching as part of the therapeutic process); professional interactions (e.g., provide constructive feedback; timely and appropriate response to feedback);
- Sufficient awareness of emotional and behavioral states to perform components, such as self-reflection, self-appraisal, and adjustment of actions when necessary (e.g., align behaviors to meet performance expectations; self-identify areas for improvement); and regulation of emotional and behavioral responses (e.g., manage uncertainty in academic and clinical/fieldwork situations; adapt thinking and behavior to changing situations).
- Participation:
a. Applicants and students must be able to participate in various experiential learning opportunities to develop the knowledge, skills, and behaviors for occupational therapy practice. Such experiential learning occurs in the classroom, laboratories, and clinical/fieldwork experiences. Students must be able to:
- Complete the interprofessional core curriculum that involves completion of online modules as well as face-to-face interactions that involve teaching, learning, and collaborating with students from various professions.
- Complete a gross anatomy course, which includes extensive hands-on dissection of human cadavers.
- Participate in classroom and laboratory activities in a co-educational environment where students are required to practice observation and intervention skills on individuals of all body types and genders. Students are often required to dress in shorts and t-shirts/sports bras to allow appropriate visualization or palpation when engaged in the simulation of patient assessment and intervention.
- Participate in small group activities and projects that require students to coordinate schedules and work collaboratively to meet assignment expectations and deadlines.
Admission to the Program
The entry-level OTD program begins in late May each year. The application for the admissions cycle opens in July. A bachelor’s degree is required prior to beginning the program. The GRE is not required for admission into the program.
The Application Process
Applicants must complete both an application through the Occupational Therapy Centralized Application Service (OTCAS) and a supplemental application. The OTCAS application and the supplemental application can be accessed through the following link: http://www.ttuhsc.edu/health-professions/admissions/application.aspx.
Applications are considered on a rolling basis for acceptance into the OTD program. The deadline for the receipt of the applications, supporting documentation, and application fee is November 15th. The application must be verified by OTCAS and the TTUHSC SHP supplemental application must be completed by the application deadline. Individual applications are only reviewed after the OTCAS verification process is completed, and the TTUHSC SHP supplemental application is submitted; therefore, it is in the applicant’s best interest to complete the application process, including submission of required documentation, as early as possible. Documentation that is required to be submitted includes transcripts, verification of observation/experience hours in occupational therapy settings, three recommendation letters, verification of required immunizations, verification of CPR certification, and personal essays. Please note: There is a time lag in submitting your application to OTCAS and the application being verified. Applicants will need to plan accordingly. It is the applicant’s responsibility to ensure all application materials have been received by OTCAS and the SHP Office of Admissions prior to the application deadline.
The selection process for the TTUHSC OTD Program is highly competitive; therefore, it is in the applicant’s best interest to complete the entire application process as early as possible. Applicants must meet the admission criteria and complete the application process prior to the deadline to be considered an eligible applicant. Many factors are considered in admissions decisions, and acceptance is offered to candidates that appear to be most highly qualified to meet the mission and goals of the OTD program. Invitations to interview with the program faculty in Lubbock, Texas are extended to the most competitive applicants. Completion of prerequisite coursework, the strength of the academic record, essays, letters of recommendation, and interviews are all strongly considered in the admissions process.
GPA Requirements
A minimum cumulative GPA of 3.0 on a 4.0 scale and a minimum Science GPA of 3.0 on a 4.0 scale are required. A competitive overall GPA and science prerequisite GPA are considerations for admissions.
Transcripts and Coursework
Applicants must submit transcripts of all institutions attended. At the time of application, the student must demonstrate the ability to complete all pre-professional coursework prior to enrollment in the first semester of the professional curriculum.
Experience
Applicants are expected to have some knowledge of the occupational therapy profession. This can be acquired in several ways: volunteer work, paid work, and/or observation in occupational therapy settings/services. It is in the best interest of the applicant to complete a substantial number of experiential hours (a minimum of 40 hours, preferably in a variety of different settings) prior to the application deadline for the program. Verification of observation/experience hours in occupational therapy practice must be submitted as a part of the application. Applicants are also encouraged to become familiar with the occupational therapy profession through exploring the professional literature and online resources.
Letters of Recommendation
Three letters of recommendation are required. One letter must be completed by an occupational therapist. Letters should be completed by professional personnel who have: (a) observed the applicant during any related volunteer, observation, or paid work, (b) been previous or present instructors and/or counselors, or (c) been previous or present employers.
Immunizations and CPR
Verification of required immunizations and CPR for the Healthcare Provider certification must be submitted prior to enrollment in the professional curriculum, or preferably by the application deadline. The program recommends CPR certification provided through the American Heart Association, as it is a common requirement for fieldwork sites. CPR certification must be maintained throughout the professional program. Immunizations will be maintained by a national database which requires an annual fee to be paid by the student.
Personal Essay
The personal essays should be submitted with the application.
Personal Interview
Competitive candidates are invited for an on-site interview during the Fall or Spring semesters. Submitting an application does not guarantee an interview.
Prerequisite Courses
The completion of the Pre-Professional Curriculum is required prior to starting the program. Courses may be completed in any regionally accredited community college, or university. All prerequisite courses must be completed prior to matriculation. It is recommended that prerequisite courses be taken within the last seven years. For the file to be reviewed, no more than 9 prerequisite hours can be in progress, and at least two science prerequisites must be completed. AP and CLEP credit will not be accepted for any science prerequisite course. There is no advanced placement, transfer of credit, or experiential learning credit within the TTUHSC OTD Program.
Below is the list of the courses that comprise the Pre-Professional Curriculum.
| Required Course | Credit Hours |
| Anatomy & Physiology (with lab) | 6-8 |
| Physics, and/or Biomechanics, and/or Kinesiology | 3 |
| Abnormal Psychology | 3 |
| Developmental Psychology | 3 |
| Statistics | 3 |